Identification of Monogenic Variants in more than Ten Percent of Children Without Type 1 Diabetes-related autoantibodies at diagnosis
Type 1 diabetes is a complex disease with insulin deficiency, certain autoantibodies and a polygenic background, whereas seemingly insulin-deficient forms of monogenic diabetes are caused by pathogenic variants (i.e. mutations) in single genes. Individuals with a subtype of monogenic diabetes (MODY, neonatal diabetes or syndromic forms of monogenic diabetes) may incorrectly be diagnosed with type 1 diabetes. The treatment of patients with monogenic diabetes can often be tailored based on the genetic diagnosis and many can use oral agents instead of insulin, as the beta cells usually preserve their ability to produce insulin.
Fig 1. Main takeaways.
This study assessed the prevalence and clinical manifestations of monogenic diabetes in the Finnish Pediatric Diabetes Register (FPDR, n= 6482) among children, who were negative for type 1 diabetes associated autoantibodies (2,3%) or positive only for low-titre islet cell autoantibodies (0,8%), and who were presumed to have type 1 diabetes at diagnosis. The FDPR covers approximately 90% of newly diagnosed diabetic individuals aged ≤15 years in Finland since 2002 and includes data on diabetes-associated HLA genotypes and autoantibodies at diagnosis.
Using a next generation sequencing gene panel including 42 genes associated with monogenic forms of diabetes, lipodystrophy, or other glycaemic traits, the researchers identified over 10% of the patients having a genetic finding as a definite or putative cause for their diabetes. Furthermore, monogenic diabetes was found in two individuals with positive low-titer islet cell autoantibodies. None of those with a genetic finding had ketoacidosis at diagnosis or carried HLA genotypes conferring high risk for type 1 diabetes.
The affected genes identified in the patients were GCK, HNF1A, HNF4A, HNF1B, INS, KCNJ11, RFX6, LMNA and WFS1. Interestingly, only a minority of the affected individuals had a known family history of diabetes.
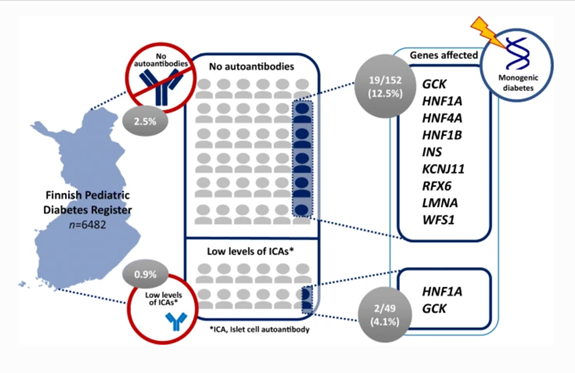
Fig 2. Visual abstract.
This study demonstrated how the correct genetic diagnosis allowed precision medicine years after diagnosis of diabetes with major benefits on glycaemic control. A switch from insulin to oral medication was successful in four of five patients with variants in HNF1A, HNF4A or KCNJ11.
This study highlights the importance of determining the autoantibody status at diagnosis of diabetes in children and adolescents and justifies testing for monogenic causes of diabetes in autoantibody-negative paediatric patients and patients with low titre islet cell autoantibodies regardless of family history of diabetes.
The study is part of a joint project between the FINNMODY study and the Finnish Pediatric Diabetes Register, led by Associate Professor Tiina-Maija Tuomi and Professor Mikael Knip. It was carried out in collaboration between HUS, the Folkhälsan Research Centre, and the University of Helsinki.
Identification of monogenic variants in more than ten per cent of children without type 1 diabetes-related autoantibodies at diagnosis in the Finnish Pediatric Diabetes Register.Harsunen M, Kettunen JLT, Härkönen T, Dwivedi O, Lehtovirta M, Vähäsalo P, Veijola R, Ilonen J, Miettinen PJ, Knip M, Tuomi T. Diabetologia. 2022 Nov 23. doi: 10.1007/s00125-022-05834-y. Online ahead of print.
